What will transplant medicine look like in the future?
Interview with Prof. Bruno Reichart, one of the leading international forces in cardiac surgery and co-leader of a consortium, which – with increasing success – is involved in the project xenotransplantation
March 2018

© Klinikum der Universität München
Thousands of people owe their lives to the cardiac surgeon Prof. Bruno Reichart. In 1983 he performed a simultaneous transplantation of the heart and lungs for the first time in the history of German surgery and became world famous overnight. On the occasion of his 75th birthday, a symposium was held at the Faculty Club G2B (Gateway to Biotech) at the IZB. Susanne Simon interviewed him for “IZB in dialog”.
Every journalist is sure to ask Bruno Reichart two questions. One concerns to the past: “How many heart transplants have you already performed in your life?” The answer: “I cannot say exactly. In Munich at the LMU, under my leadership, there were more than a thousand, but of course I did not perform all of them myself. In Cape Town at the Groote Schuur Hospital, one can likely add about one hundred more.” The other question concerns the future of medicine: “When will the first human live with a pig’s heart?” Reichart’s prognosis: “I know that this is possible with non-human primates. To bring the method to the clinic, certain conditions must be met – and that will take at least three years, at best.”
Bruno Reichart, born in Vienna and growing up in Ingolstadt, first studied in Erlangen and then at the LMU, where he has spent more than 40 years off and on. He began his clinical career with Prof. Zenker in general surgery, and then soon switched to cardiac surgery with Prof. Klinner. In 1984 he became the successor to Christiaan Barnard at the University of Cape Town. He was head of LMU cardiac surgery from 1990 to 2011, then spent four years as spokesman for the special research area Transregio “Xenotransplantation”, a DFG-funded research collaboration with the goal of successfully transplanting pig tissue and organs into primates. He is currently the co-speaker of this consortium, after handing over the leadership to Eckhard Wolf, Professor of Molecular Animal Breeding and Biotechnology at the Gene Center of LMU. Reichart’s research is running at full speed, his labs with surgery facilities are housed in the Walter Brendel Institute of the Grosshadern Clinic. The team also includes two ethicists and one legal expert.

© Klinikum der Universität München
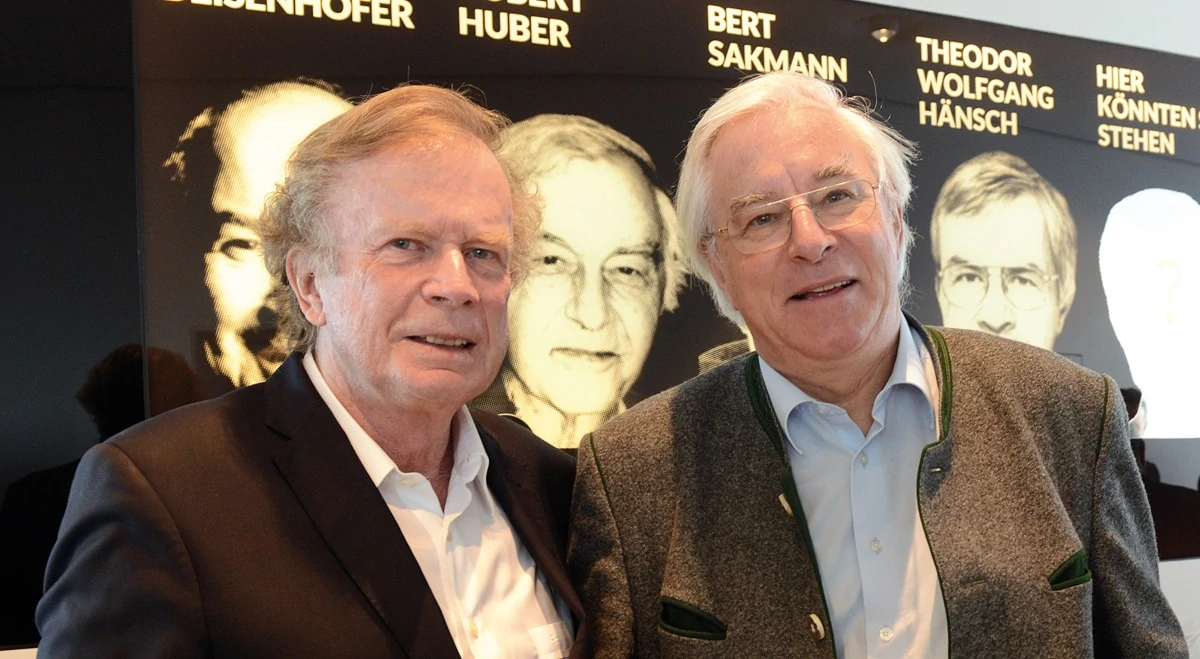
Dr. Peter Hanns Zobel, Geschäftsführer / CEO, IZB, Elke Reichart, Prof. Bruno Reichart (v.l.n.r.)
in Dialog: The „Who is Who“ of heart specialists met at the symposium organized on the occasion of your birthday. A highly interesting event that particularly looked forward to the future – not exactly to be expected for a 75th birthday?
Prof. Reichart: The symposium was organized without me. A very nice event indeed. The dean of the Medical Faculty, the Medical Director of the Clinic Großhadern and my current team participated. Also many colleagues from the last 40 years, from clinical times, as well as from the years of intensive research in the field of xenotransplantation, had come, for example from the different locations of the Transregio: from Hanover, Dresden, Langen, Berlin and Munich, as well as Bern and Geneva.
”Future xenogenic heart transplantation in humans can be scheduled and need less immunosuppressive drugs.”
Prof. Bruno Reichart

Transplantation medicine has always had a big problem: there are not enough donors for the many patients who could benefit from organ transplants. Transplantation not only extends the life of the terminally ill, but also provides a better quality of life.
© Klinikum der Universität München
in Dialog: Why is your focus on xenotransplantation, which for many people is still an exotic field of research?
Prof. Reichart: Transplantation medicine has always had a big problem: there are not enough donors for the many patients who could benefit from an organ transplant. Transplantation not only extends the life of the terminally ill, but also provides a better quality of life.
In Germany, this donor shortage was always particularly pronounced, and the crisis has currently reached a peak: in 2017, the number of donors fell below ten in a million people. Actually, this means Germany should no longer be a member of Euro transplant.
Of course, the specialist societies and the German Medical Association have to work on possible solutions, for example on changing the logistics. In addition, a well-functioning alternative to human transplantation would be extremely important – and now we are back to the theme of xenotransplantation. Xenos is Greek and means „foreign“. In this case the word refers to non-human species whose tissues and organs are transplanted. It would be easiest to use non-human primates – monkeys – as donors. Indeed, I did carry out preliminary experiments with baboons and green monkeys with my team in Cape Town back in the 1980s. We were successful, but discontinued due to objections from the university and society at the time. Tissues and organs from species far removed from the primates are more likely to be accepted, so the choice was pigs. Some people turn up their noses because they think pigs are an unclean species. It should be remembered that about 90 million years ago pigs were the most highly developed mammals on the planet and so we have common ancestors.
© Klinikum der Universität München
Prof. Bruno Reichart , Prof. Dr. med. Karl-Walter Jauch, Chairman of the Executive Board Grosshadern Clinic.

© Klinikum der Universität München
Prof. Paolo Brenner, Heart Surgery at the LMU, delivers a talk to the symposium
in Dialog: How do you avoid rejection reactions after xenotransplantation?
Prof. Reichart: The huge difference in developmental history means that one cannot simply transplant tissue and organs from untreated pigs into primates and ultimately humans – the result would be hyperacute rejection and coagulation disorders such as thrombosis. The appropriate pigs must therefore be genetically modified: harmful genes are removed from the genome, and certain human genes are added. This is the task of the veterinarians, we – the pre-clinicians – must ensure that the transplanted tissues (such as the islets of the pancreas, or heart valves) and organs (hearts and kidneys) work for a long time in primates. Both are not easy and many things have to be accomplished for the first time.
In dialog: What is the current state of research in transplantation medicine?
Prof. Mayerle: The Dresden group of Dr. med. Barbara Ludwig and Prof. Stefan R. Bornstein have macro-encapsulated the islets of the pancreas. The capsules are implanted under the skin – you can think of this as a pacemaker, except that in this case the surrounding porous membrane allows the small glucose molecules in the blood to reach the islets, which then results in the release of adequate amounts of porcine insulin. The nice thing is that the surrounding porous membrane has such small holes that rejection mechanisms such as antibodies and cells cannot get inside the capsule. Therefore, you need no immunosuppression and the donor pigs do not have to be genetically modified. The Dresdner Group wants to start a pilot project in 2018 with eight diabetic patients.
The Munich-based group led by Jochen Seissler from the LMU Med IV in the city center prefers the transplantation of non-encapsulated islets, which then have to be genetically modified and also require immunosuppression. Organs cannot be encapsulated anyway.
Recently, we have achieved real and consistent long-term success with porcine heart replacement in non-human primates – results that have never been achieved before. So the prospect of a clinical application has moved almost within reach. Future xenogenic heart transplantation in humans can be scheduled, i.e. performed during the day, during the best working hours. The microbiological state of health of the genetically modified pigs will also be known, in other words: no infections will be transmitted, which are sometimes a problem in human transplants, since these procedures often have to be carried out under severe time pressure.
in Dialog: What will transplantation of the future look like?
Prof. Reichart: As I said, to reach the clinic we will still need time – and also investments. If you ask me about my dream, which in my opinion is not so unrealistic: the transplanted tissues and organs will in the future be genetically programmed to also carry an immunosuppressive molecule on all their cells, so that even fewer corresponding drugs are needed – or perhaps none at all. We are already working on this solution.

© Klinikum der Universität München
Guests of the symposium on xenotransplantation
(v.l.n.r.) 1st row: Prof. Robert Rieben (exp. Chirurg Bern), Dr. Tanja Mayr (Konsortium Xenotransplantation München), Dr. Andrea Bähr (exp. Kardiologie TU München), Elke Reichart, Dr. Daniel Reichart (Kardiologie UKE Hamburg), Prof. Bruno Reichart, Dr. Raffaela Schwarzkopf-Ehrl (Leiterin Juristisches Referat LMU), Prof. Paolo Brenner (Herzchirurgie LMU), Prof. Ernst-Ludwig Winnacker (Genzentrum LMU)
2nd row: Dr. Ralf Tönnjes (Paul-Ehrlich-Institut Langen), Prof. Michael Schmöckel (Herzchirurgie Asklepius Hamburg), Prof. Bernd Kemkes (ehem. Herzchirurgie München-Bogenhausen), PD Peter Lamm (Herzchirurgie Artemed München), Dorothea Marquardt (Konsortium Xenotransplantation München), Prof. Reinhard Hickel (Dekan med. Fakultät LMU), Prof. Klaus Peter (Alt-Dekan med. Fakultät LMU), Dr. Rabea Hinkel (exp. Kardiologie TU München), Prof. Bruno Meiser (Leiter Transplantationszentrum LMU)
3rd row: Dr. Matthias Längin (Anästhesie LMU), Prof. Ralf Sodian (MediClin Herzzentrum Lahr/Baden), Prof. Christian Hagl (Herzchirurgie LMU), Prof. Theodor Fischlein (Herzchirurgie Nürnberg), Dr. Joachim Denner (Robert-Koch-Institut Berlin), Angelika Schmid (München), Prof. Karl Jauch (Ärztlicher Direktor LMU), Dr. Jan Abicht (Anästhesie LMU), Dr. Peter Murray (Max-Planck-Institut Martinsried)
4th row: Prof. Bernd Zwissler (Anästhesie LMU), Prof. Peter Überfuhr (ehem. Herzchirurg LMU), Dr. Ferdinand Vogt (Herzchirurgie Nürnberg), Prof. Jochen Seissler (Med. IV LMU), PD Sebastian Michl (Herzchirurgie LMU), Prof. Angelika Schnieke (Lehrstuhl Biotechnologie der Nutztiere TUM), PD Gerd Juchem (Herzchirurgie LMU), Prof. Reinhard Schwinzer (Transplantationsimmunologie Hannover), Prof. Eckhard Wolf (molekulare Tierzucht und Biotechnologie am Genzentrum München)
5th row: Toni Schmid (Bayerisches Kultusministerium), Prof. Alex Kind (Biotechnologie der Nutztiere TUM), Dr. Christian Epp (Dekanat med. Fakultät LMU)
last row: PD Nick Klymiouk (molekulare Tierzucht und Biotechnologie am Genzentrum München), Prof. Jörg Seebach (Klinik für Immunologie und Allergologie, Universität Genf)
- Marchioninistraße 15
- 81377 München
- Phone: +49 (0)89/4400 – 72101
- ed.nehcneum-inu.dem@greb.aidualc
- www.klinikum.uni-muenchen.de